TENNIS INJURIES
Tennis Injuries
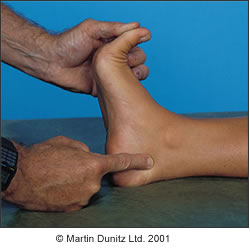
Lateral Ankle Sprains
Tennis is a multidirectional sport that comes with a great degree of lateral moment, specifically as the athlete’s eyes are on the ball and often not watching their foot placement. The running, jumping and landing involved (even when serving the ball) in tennis can result in landing incorrectly turning the ankle over. It is good to be mindful that clay courts are slippery but also soft, so the lateral aspect of the foot can dig into the ground upon landing, inverting the foot and significantly increase the risk of an ankle sprain.

Tennis Toe ie Subungual Haematoma
Tennis toe is caused by repeated pressure or injury to the toenail causing pooling of blood under the nail. A Subungual Haematoma is common in tennis as the big toe especially is used to drag on the ground during a serve or play, as well as the “stop and start” nature of the game, causing the toe to glide towards and hit the end of the shoe. Often however this injury is primarily caused by shoes that are too short, or narrow at the toebox, so make sure you get fitted professionally into tennis shoes as well as keeping the toenail clipped short to avoid this issue. If your big toe goes “up at the end” and commonly hits the top of your shoe, come into the clinic for a Musculoskeletal assessment to look at options to reduce the hyperextension of the big toe joint.
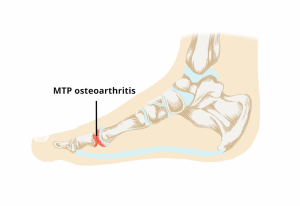
Sesamoiditis
The sesamoids are two small spherical bones underneath the base of your big toe, encased by the big toe’s flexor tendons that stabilized the big toe joint when flexed. Tennis players spend a lot of time on the toes to be ready to move quickly in response to game play quickly as well as landing on the toes a lot which places the joint in a flexed position under a lot of body weight. Repeated strain to the big toe joint in this position can cause the Sesamoid bones to be inflamed and in serious cases, fracture.
Plantar Fasciitis or Plantar Heel Pain
Tennis is a sport played on hard surfaces in firm shoes. Although there are many Biomechanical factors that more commonly predispose someone to have Plantar Fasciitis, ie the inflammation of the long fascia band (a crucial tissue in the foot that is similar to muscle tissue) that connects at the heel, hard surfaces can contribute to symptoms if there is an existing heel pain caused by Plantar Fasciitis. It is important to see your Podiatrist to get these contributing factors addressed as this condition can become quite recalcitrant if left untreated.
Peroneal Tendinopathy
The Peroneal musculature involves 3 muscle tendons running to the outside of foot, which when inflamed through Tendinopathy cause pain commonly to the lower lateral ankle but mostly to the lateral border of the foot. The Peroneal muscle group’s role is to evert or pronate the foot, and is often active as a reaction during an ankle sprain or excessive lateral load to take the foot out of the “rolled” or vulnerable position by rolling the foot in. In tennis, players have to rely on loading the lateral foot in change of direction, which can create overuse to the Peroneals and eventuate in injury over time.
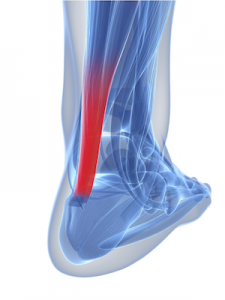
Achilles Tendinopathy
A common overuse injury caused by microtrauma to the tendon described as pain, swelling and stiffness to the tendon either at its join at the back of the heel or towards the calf region. Achilles Tendinopathy is prevalent in tennis due to the major loads placed on the calf muscle in short bursts of movement (deceleration and acceleration) in game play and during hitting a forehand or a backhand by use of an open stance, which places a majority of the stress on the calf during the backswing. In serving, stress is also placed on the calf and achilles during a ball toss. It is important to rehabilitate this condition before continuing to play, as if the tendon is inflamed in some cases it can rupture or tear without intervention if repeated microtrauma is sufficient enough.
Cramping
Muscle cramping, commonly in the calf or sole of the foot, occurs when there is a reduced blood supply to the area and in tennis is often due to an increased loss of bodily fluids due to sweating in exercise.
Muscle cramps can be quite debilitating and frustrating, preventing a player from continuing in a match or reducing movement.
Preventing cramping
Ensure cool clothes to reduce body temperature, drink electrolytes, ensure good training and strength and conditioning incorporated into training and prepare for long matches.
Blisters
The main cause of blisters in tennis is a combination of friction and shear. In tennis due to the combination of both running and pivoting on the feet, the skin is pulled in different directions, and this is known as “shear” force.
Preventing blisters
A tight fitting anatomical sock is best to reduce the likelihood of skin movement. Moisture wicking fibres are also helpful as the skin is more likely to break down into a blister when the foot is sweating.
Injury Prevention Tips
Warm Up
Warming up especially before competitive tennis is crucial to prepare the body for the more strenuous nature and demands of competitive play. Tennis is a game that although has times of rest between points, is no less difficult and can be very gruelling and harsh on the body in longer game times!
Shoes
Injury prevention? This is where appropriate shoes come into play. For tennis, if you are training once a week or more or playing matches or competitively at all you should definitely be wearing a shoe that is appropriate for the sport-a tennis specific shoe. Tennis shoes are categorised often into hard court, clay shoes or grass shoes.
Tennis shoes are structured to provide:
- Rigidity to the midfoot and heel of the shoe to reduce the likelihood of unwanted torsion (rotation) through the foot, thus enhancing stability of the ankle in comparison to a pair of runners.
- Allowance for lateral movements (side to side movement)
- Panelling in the upper material that is more rigid around heel and midfoot to secure the ankle in place better
- A toe guard at the toe box to protect the mesh upper from getting damaged during a drag/slide or toe pressure from inside the shoe.
- A hard court shoe is heavier, giving the shoe’s outsole durability and cushioning for hours on the more unforgiving surface
- A herringbone or Entecar sole allows for the best grip on your surface whilst allowing a slide/drag if needed on a clay/Entecar court.
Surfaces
- If you can play on Clay or Grass, this is ideal for prevention of stress related or joint injuries as the surface is much softer and easier on the joints and feet!
- However, if you are prone to ankle sprains, for example, a hard tennis court is better in assisting you to grip your surface better compared to the more slippery nature of a clay or grass surface.
- Before starting to compete or play matches, make sure you are familiar with the court surface you will be competing on.
Blisters
- Check your feet for bony protrusions
- Shake your shoes out especially after play on clay to avoid debris causing pressure areas on the feet during play
- Lace up your shoes just right
- Wear in new shoes gradually-ie walk around in your new tennis shoes first, then train in them, before playing a match
If you play tennis and have any injury even if experiencing different symptoms to the above common conditions, please book in with one of our Podiatrists for a Musculoskeletal assessment where we will form a comprehensive treatment plan so you can get back to the court as soon as possible!