Surfcoast Trek Total Care Podiatry
The Surfcoast Trek is scheduled for Saturday 2nd April 2022 and Total Care Podiatry is proud to continue its association with such a wonderful event.
Check out https://surfcoasttrek.com.au/the-trek if you have not heard of this event that aims to take walkers on the beautiful Great Ocean Road Walk from Anglesea to Torquay.
A number of distances are scheduled so based on your capabilities select you distance and get training. This is a major fund raising event for Kids+ and Give where you live foundation.
The three stages we are involved are before, during and after the event.
Before the Trek
I hope everyone is thinking about their training load, socks, clothing and footwear.
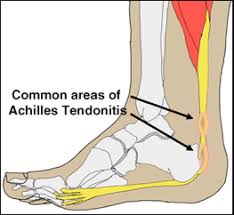
Training load – increase your training load by no more than 10% per week and seek help from our Podiatrists if you experience foot pain.
Socks – select a sock that is your size, is at least 70% natural fibre and will not fall down during the walk. We love Injinji, Wigwam and OS1st for compression base layer. Visit an outdoor hiking shop for hiking socks and don’t be cheap!
Clothing – hiking shorts or pants for all conditions, think sun and rain
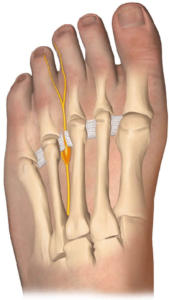
Footwear – Hiking boot, Hiking shoe, trail runners or trail shoe. This can be a confusing choice. If you plan to carry a day pack then a hiking boot gives you added stability in the ankle when walking on uneven terrain in the event you stumble. A boot just might save your ankle as it is very hard to save yourself once you stumble with the added weight of a pack. Hiking shoes shall be the most popular as they have a sturdy out sole to protect the foot from stone strike. They are very roomy in the toe box as the foot and toes will swell on a longer hike and accomodate this and a thicker hiking sock. Now is the time to visit a hiking shop to get your hiking shoes fitted if you don’t already have a pair you just love. Trail runners will provide a little more protection from stone strike than a standard runner. If you are considering wearing runners then make sure you have done plenty of walking on non sealed surfaces.
Total Care Podiatry are providing a 10 minute free consultation before the event to all participants who are registered for the 2022 event. This consultation will be for advice and if treatment or further care is recommended fees will apply. This is available at 209 Malop St Geelong.
During the Event
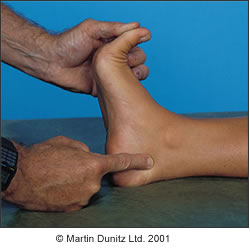
Total Care Podiatry will be providing foot care during the event to participants who experience blisters, foot pain and or tendon issues. Our Podiatrists will be available at the starting point and then at each check point along the way and the finish line. We will have dressings, strapping and advice on hand to assist with your foot complaints. The majority of complaints on the day are blisters.
After the event
If you develop a problem during or after the event then please follow up with Total Care Podiatry for advice and treatment. Normal fees apply for consultation after the event.
Total Care Podiatry has very experienced Podiatrists who have walked these distances and more so are in an ideal position to treat and recommend solutions to your walking related foot problems.
Call the clinic on 03 5223 1531, email us or make an online booking for further advice.

Wigwam Socks and Hiking Shoes

Hiking shoe with a rocker sole to reduce foot fatigue

Consider walking poles. Philip Spark loving them on steeper longer walks.

Make sure your shoes are not too warn out. I lost the left vibram sole and had to walk out 4 hours. I felt every stone.