EXPERIENCING PAIN IN YOUR ANKLES, KNEES OR HIPS?
At Total Care Podiatry the podiatrist will ascertain what dysfunction is occurring in your feet, how this is interacting with the muscles in your back, pelvis and legs and will see what areas in your lifestyle may be placing you at risk of continuing the injury. We will also work together with other health professionals involved in your care to achieve a long term solution.
Your knees and hips are the largest joints in your body. They are responsible for supporting your weight as you stand and walk. If you are experiencing chronic pain in your hips, knees, or even in your lower back, shoulders and neck, there may be a connection between this pain and the way your feet function.
Walking is good for you, right? Absolutely. But beware of poor walking habits that can cause or exacerbate knee and hip problems. On the positive side, however, a safe and smart walking regime can help improve joint problems, not to mention how good it is for your overall health.
KNEE PAIN
Watch your feet. If you are prone to foot problems, such as hypermobile feet (when the joints in and around the feet move more than they should) or fallen arches caused by over pronation, your gait may be compromised. And this change can cause unnecessary stress on the knees, resulting in painful injuries.
The knee is made to bend only in one direction—facing straight forward. When the foot over-pronates, the leg rotates inward toward the opposite leg. This causes the knee to flex and extend while pointing inward and not in the normal direction, which puts stress on the knee.
People who suffer from osteoarthritis pain have worn cartilage on the inside (medial) area of their knee joint. Research is being done to determine how walking differently can help manage this pain. According to the Arthritis Foundation, studies are finding that pointing your toes slightly outwards (about 7°) when you walk will shift pressure to the outside (lateral) part of the knee, relieving the pain radiating from the inside of your knee joint.
RUNNER’S KNEE (which is not exclusive to runners!) is identified by a throbbing pain on your kneecap. The impact of your foot hitting the ground causes your kneecap to rub against the femur bone. If you have a misaligned kneecap or previous injury, your knees are more vulnerable. Other causes are weak thigh muscles, soft knee cartilage, or flat feet.
HIP PAIN
Pain from bursitis is felt on the outside of your hip, whereas arthritis is felt on the inner hip near your groin. Relief from each requires different walking treatments.
Repetitive stress (including excess walking or running) can cause the bursa that cushions your hip to become inflamed. Another cause of bursitis is exercising without proper warm-ups and cool downs, which are a vital part of any program. You need to follow a very slow walking regime when recovering from a bout of bursitis. This involves gradually increasing the frequency and length of your walks.
As with osteoarthritis in general, the cause of hip arthritis can be genetic. It can be a hereditary or a congenital problem with an improperly formed hip joint. Hip arthritis can also develop from an injury or trauma to the hip area, or stress from excess weight or activity.
The problems caused by over pronation, which were discussed for knee pain, are also true for the hip joint. When the foot pronates, the leg rotates inward and the hip can become unaligned. This condition puts stress on the hip and on the entire leg muscles.
HOW TO HELP YOUR ANKLES, KNEES AND HIPS
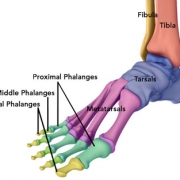
Any problem with the foot or ankle resulting in a compromised posture or gait can lead to knee and hip pain. Examples of common foot problems that can lead to poor posture and irregular walking patterns include:
- Plantar fasciitis, which can lead to chronic heel pain and/or arch pain
- Nerve pain or numbness in the foot (such as neuromas and tarsal tunnel syndrome)
- Bunions and bunionettes (big-toe versus little-toe side, respectively)
- Excessive foot pronation (rolling in) or supination (rolling out)
When you experience pain and you are diagnosed with a dysfunction in the foot or ankle, it may be possible to reduce the knee and hip pain by improving foot function, using proper footwear and orthotic insoles.
A Harvard medical school health publication advises that exercise is an important treatment for arthritis. It improves the strength and function of the afflicted area(s).
In many cases, a moderate walking plan is recommended to alleviate such pain. It is considered a low impact activity that strengthens the supporting muscles, relieving the pressure on the joint. Be sure to walk on a smooth, soft surface such as a track or treadmill. Your doctor or physical therapist can advise how much walking is best for you. An extra bonus is walking will help with weight loss, which takes some stress off your joints.
When you compensate for pain by limping or walking with an abnormal gait, other joints can suffer wear and tear. Your rheumatologist, orthopedic doctor or physical therapist can help determine if changing your walking gait could help reduce pain. Many PTs will video patients as they walk on a treadmill and then review their walking habits to determine what pain reduction improvements can be made. You can make a conscience effort to minimize limping by holding your body straight without swaying and maintaining and even stride.
THE RIGHT SHOE REGIME
Healthy shoes play a significant role in knee and hip pain management. Here are a few tips on the importance of wearing good shoes.
- Never wear heels over two inches high. Heels increase the risk of knee joint degeneration.
- However, not all flat shoes are good for your feet. Flats that do not provide any arch support can lead to knee, hip, and back pain.
- Get the right fit. Tight shoes can cause limping from foot pain. Oversized shoes can also impair your gait. Either way, you’ll be putting unnecessary stress on your knees and hips.
- Stability sneakers provide cushioning and help control over pronation. They also relieve the ball of the foot, which helps arthritic pain in the hip, knee, foot or ankle.
- Replace your shoes as needed. When the supporting cushioning becomes worn, it is no longer helpful.
- If knee or hip pain is due to your foot function, the proper footwear along with orthotic insoles can be a very effective way to relieve symptoms.
- Invest in quality shoes that are specifically made for your condition. Total Care Podiatry provides the ability to browse shoe selections that meet your needs.
At Total Care Podiatry the podiatrist will ascertain what dysfunction is occurring in your feet, how this is interacting with the muscles in your back, pelvis and legs and will see what areas in your lifestyle may be placing you at risk of continuing the injury. We will also work together with other health professionals involved in your care to achieve a long term solution.
WARNING
THIS INFORMATION IS FOR EDUCATIONAL PURPOSES ONLY AND IS NOT INTENDED TO REPLACE PROFESSIONAL PODIATRIC ADVICE. TREATMENT WILL VARY BETWEEN INDIVIDUALS DEPENDING UPON YOUR DIAGNOSIS AND PRESENTING COMPLAINT. AN ACCURATE DIAGNOSIS CAN ONLY BE MADE FOLLOWING PERSONAL CONSULTATION WITH A PODIATRIST.